Abstract
Objective
To investigate the relationship between ambient temperature and atmospheric pressure (AP) and the severity of heart failure (HF) decompensations.
Methods
We analysed patients coming from the Epidemioloy Acute Heart Failure Emergency (EAHFE) Registry, a multicentre prospective cohort study enrolling patients diagnosed with decompensated HF in 26 emergency departments (EDs) of 16 Spanish cities. We recorded patient and demographic data and maximum temperature (Tmax) and AP (APmax) the day before ED consultation. Associations between temperature and AP and severity endpoints were explored by logistic regression. We used restricted cubic splines to model continuous non-linear associations of temperature and AP with each endpoint.
Results
We analysed 16,545 patients. Daily Tmax and APmax (anomaly) of the day before patient ED arrival ranged from 0.8 to 41.6° and from − 61.7 to 69.9 hPa, respectively. A total of 12,352 patients (75.2%) were hospitalised, with in-hospital mortality in 1171 (7.1%). The probability of hospitalisation by HF decompensation showed a U-shaped curve versus Tmax and an increasing trend versus APmax. Regarding temperature, hospitalisation significantly increased from 20 °C (reference) upwards (25 °C: OR = 1.12, 95% CI = 1.04–1.21; 40 °C: 1.65, 1.13–2.40) and below 5.4 °C (5 °C: 1.21, 1.01–1.46). Concerning the mean AP of the city (anomaly = 0 hPa), hospitalisation increased when APmax (anomaly) was above + 7.0 hPa (atmospheric anticyclone; + 10 hPa: 1.14, 1.05–1.24; + 30 hPa: 2.02. 1.35–3.03). The lowest probability of mortality also corresponded to cold-mild temperatures and low AP, with a significant increased risk only found for Tmax above 24.3 °C (25 °C: 1.13, 1.01–1.27; 40 °C: 2.05, 1.15–3.64) and APmax (anomaly) above + 3.4 hPa (+ 10 hPa: 1.21, 1.07–1.36; + 30 hPa: 1.73, 1.06–2.81). Sensitivity analysis confirmed the main analysis results.
Conclusion
Temperature and AP are independently associated with the severity of HF decompensations, with possible different effects on the need for hospitalisation and in-hospital mortality.
Similar content being viewed by others
INTRODUCTION
Climate change is expected to increase the frequency and intensity of extreme meteorological conditions, in a scenario in which severe cold weather may anomalously alter warm temperatures in winter, whereas heat waves may become more intense from spring to autumn.1 This scenario represents a threat to public health, since increases in mortality by cardiovascular and respiratory diseases are typically observed during both hot and cold weather conditions.2,3 Among cardiovascular diseases, extreme temperatures have been associated with increased risk of myocardial infarction as well as larger infarct size.4–6 On the other hand, a failing heart is one of the leading cardiovascular causes of death associated with extreme ambient conditions, and in this context, individuals with heart failure (HF) are likely to be unable to compensate for the increased circulatory demand induced by heat exposure.7
Heart failure (HF) is a highly prevalent cardiovascular condition in people over 65 years old.4,5 Mortality associated with HF decompensations (acute HF, AHF) is high, with in-hospital all-cause mortality ranging from 5 to 10%.6,7 Many variables related to patient baseline characteristics and to the acute episode of decompensation with potential to predict such adverse outcomes have been unequivocally defined.6–10 Conversely, the importance of meteorological conditions on the immediate prognosis of patients with AHF has been poorly investigated. Many previous reports are epidemiological studies based on time-series analysis in general populations investigating the incidence of certain cardiovascular diseases, such as acute coronary syndrome,11 or the overall or cardiovascular patterns of mortality related to meteorological conditions. However, these studies mainly focus on the effect of high temperatures in hot regions of the world, or analyse the impact on mortality during heatwave episodes. Alahmad et al. recently reported a threefold increased risk of cardiovascular mortality during periods of maximum risk temperature (42.7 °C) with respect to those of minimum risk temperature (34.7 °C) in Kuwait.12 Remarkably, no previous study has analysed the severity of decompensations and the risk of adverse events for AHF, and neither has the effect of atmospheric pressure (AP) on top of the effect of temperature been investigated. Therefore, we aimed to investigate the relationship between ambient air temperature and AP and the severity of HF decompensations.2,3
METHODS
Setting, Study Design and Patient Inclusion
This study is a subanalysis of the Epidemioloy Acute Heart Failure Emergency (EAHFE) Registry,13 a prospective, multicentre, cohort study initiated in 2007 (see supplementary material). The authors designed the study and gathered and analysed the data according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (Supplementary Table 1).
Exposure Variables
The primary exposure variables of interest were the daily values of maximum temperature (Tmax) and maximum AP (APmax) for the day before patient consultation to the ED. Maximum temperature and pressure were chosen the day before ED consultation in order to ensure they had an effect on the severity of decompensation (as those registered on the day of ED consultation could not affect patients arriving to the ED early in the morning). These meteorological variables were recorded by the Meteorological State Agency at stations near the hospital. We compiled Tmax in degrees Celsius (°C) and APmax in hectopascals (hPa). The AP is a meteorological variable which decreases with altitude, and therefore, cities located at sea level have a higher mean AP than those located at a higher altitude (i.e., the mean AP is 1018 hPa in Barcelona, located at 13 m above sea level, and 917 hPa in Burgos, placed at 859 m above sea level; see Fig. 1), The statistical analysis was performed using the anomaly of the APmax [APmax (anomaly)] for each day. The concept of APmax anomaly was used and calculated in a similar way as that used in many climate studies: APmax anomaly (for day d) was obtained as the result of the average value of APmax during a certain period (in the current study, the APmax of all days included in the study) minus the value of APmax of day d. Accordingly, a day with an APmax (anomaly) equal to zero means that the APmax was equal to the mean APmax in that city; similarly, a negative value means a day with a low APmax and a positive value represents a day with a high APmax for every particular city. These negative and positive APmax values are generally associated with changes in weather, i.e. the passage of a cyclone (or depression or heat low) for negative APmax or an anticyclonic weather situation for positive APmax values. In Spain, the day-to-day variability in temperature and AP is regularly associated with the shifting of the Azores anticyclone and mid-latitude depressions/cyclones.
Covariates
We considered demographic factors including age, sex, and 6 clinical risk factors: diabetes mellitus, hypertension, coronary artery disease, chronic renal disease, cerebrovascular disease, and chronic obstructive pulmonary disease. These comorbidities have been considered to impact prognosis in general as well as in previous studies analysing the effects of temperature on mortality. We also considered three demographic data consisting in day of the week and season of the year of patient arrival to the ED (there were no inclusions in the summer due to logistic issues—vacation time of most of ED staff; the EAHFE Registry never includes summer periods for patient recruitment) and the climate type of the city where the ED is located according to official Spanish climate data.14
Outcomes
We considered two different outcomes to assess the severity of the AHF episode: (1) need for hospitalisation (accounting for every patient who, after ED evaluation and treatment, required hospitalisation, irrespective of the department in charge of the admission) and (2) in-hospital all-cause mortality.
Statistical Analysis
Continuous variables are expressed as mean and standard deviation (SD) or median and interquartile range (IQR), and categorical variables as absolute values and percentages. Confidence intervals of proportions were computed using the Wilson method.15 Binary logistic regression analysis was used to investigate the potential association of Tmax and APmax (anomaly) with each outcome. To avoid dichotomizing Tmax and APmax (anomaly) into a few discrete, ordered levels and to avoid imposing linearity, we used a restricted cubic spline function to model the continuous association of Tmax and APmax (anomaly) with each outcome. Four spline knots were placed at the 0.05, 0.35, 0.65 and 0.95 percentiles of each continuous variable marginal distribution, following the recommendations of Harrel.16 Adjustment was performed for age, sex, patient comorbidities, demographic data (day of the week, season of the year and city climate) and daily Tmax and APmax (anomaly). The magnitude of the effect of each Tmax and APmax (anomaly) unit change was graphically assessed. Because both continuous variables were modelled with restricted cubic splines, their adjusted associations were expressed in a dose-response manner for probability or odds ratio (OR) with 95% confidence intervals (CI) for each outcome of interest. In order to compute an OR for the dose-response plots, we chose a priori a Tmax of 20.0 °C and an APmax (anomaly) of 0 hPa as the reference values. These reference values were chosen arbitrarily, as there are no previous studies suggesting any theory-based reference value for temperature and atmospheric pressure in patients with AHF. Two-dimension plots (heat maps) were constructed to assess the relationship between Tmax and APmax (anomaly) for each endpoint.
Two sensitivity analyses were performed to assess the robustness of the main analysis: first, we included an interaction between temperature and AP in the multivariable model used for the main analysis (sensitivity analysis A), and second, we adjusted for chronic HF as an additional covariate in the main multivariable model (sensitivity analysis B). In addition, we performed a subgroup analysis based on the four climates (Mediterranean, continental, oceanic or subtropical) in the cities studied.
All hypothesis testing was two-tailed, and p values < 0.05 or ORs 95% CI excluding 1 were considered statistically significant. All analyses were performed using observed cases without imputation of missing data due to the extremely low missing rate (0.25%). Data analysis was performed using Stata version 16.1 (Stata Corp, College Station, TX, USA) and R version 3.6.3 (R foundation for Statistical Computing, Vienna, Austria).
RESULTS
Characteristics of Patients, Temperature and Pressure
A total of 16,447 patients with AHF were available for this analysis (Supplementary Figure 1). The median age was 83 years, 56% were women, and the most frequent comorbidities were hypertension and diabetes mellitus (Table 1). ED consultation was more frequent during weekdays than during weekends, and a higher proportion of patients (68%) were included in winter. Most patients were attended at the EDs of Mediterranean and continental cities, whilst less than 15% corresponded to EDs of cities with an oceanic or subtropical climate (Table 1).
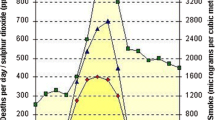
The mean Tmax and APmax the day before patient arrival to the ED were 16.4 °C (range: 0.8 to 41.6) and 983.0 hPa (range: 892.1 to 1036.7), respectively. After APmax transformation, the mean APmax (anomaly) was − 0.2 hPa (range: − 61.7 to 69.9) (Fig. 2).
Association of Temperature and Atmospheric Pressure with Hospitalisation
Hospitalisation was necessary in 12,352 HF patients with decompensation (75.2%; this data was unknown in 12 cases). The expected probability of hospitalisation due to HF versus Tmax exhibited a U-shaped curve, with lower probabilities with a Tmax between 10 and 20 °C (minimum probability at Tmax at ~ 16 °C, Fig. 3), and cold and warm temperatures significantly increasing the need for hospitalisation. Specifically, with respect to a temperature of 20 °C (reference), hospitalisation significantly increased above this point (for 25 °C: OR = 1.12, 95% CI = 1.04–1.21; 30 °C: 1.27, 1.07–1.52; 35 °C: 1.45, 1.10–1.91; 40 °C: 1.65, 1.13–2.40) as well as below 5.4 °C (5 °C: 1.41, 1.17–1.71) (Fig. 3 and Table 2).
Adjusted effects of temperature and atmospheric pressure on the need for hospitalisation of patients with AHF. Upper panels correspond to restricted cubic spline curves for predicted probabilities, and middle panels correspond to the odds ratio of hospitalisation for every temperature and atmospheric pressure value, choosing as reference a temperature value of 20 °C and an atmospheric pressure value of 0 HPa. The bottom panel corresponds to the heat map for probability of hospitalisation according to temperature and atmospheric pressure [inside, dot plot including the whole range of temperatures (from 0.8 to 41.6 °C) and atmospheric pressure anomalies (from − 61.7 to 69.9 hPa)]. The multivariable regression model was adjusted for median age (82 years), gender (reference Female), weekday (reference Monday), season (reference Winter), climate (reference Mediterranean), hypertension, diabetes mellitus, chronic kidney disease, coronary heart disease, cerebrovascular disease, and chronic obstructive pulmonary disease (for all risk factors, the reference was No).
The probability of hospitalisation rose with increasing APmax (anomaly). In this sense, with respect to the mean APmax of the corresponding city [0 hPa of APmax (anomaly)], hospitalisation significantly increased when the APmax (anomaly) was above + 7.0 hPa (anticyclonic condition; + 10 hPa: 1.14, 1.05–1.24; + 20 hPa: 1.52, 1.20–1.91; + 30 hPa: 2.02, 1.35–3.03) (Fig. 3 and Table 2). Sensitivity and subgroup analyses showed very similar results compared to the main analysis (Table 2 and Supplemental Figures 2, 3 and 4).
The contour plot (Fig. 3) shows that the probability of hospitalisation due to HF decompensation was (1) minimum (< 68%) when the Tmax was mild (12–19 °C) and the APmax (anomaly) was negative (~ − 20 hPa), a scenario frequently associated with southern warm winds in autumn and spring linked to an approaching cyclone from the Atlantic, and (2) high (~ 75–80%) when the Tmax was low (< 5 °C) and the APmax (anomaly) was positive (> 7 hPa), a typical scenario of cold weather linked to anticyclonic conditions in winter, often associated with inversions near ground level and fog, and (3) is maximum (80%) when the Tmax is high (> 30 °C), irrespective of the APmax (anomaly), a typical scenario of hot weather in early autumn and the end of spring.
Association of Temperature and Atmospheric Pressure with In-Hospital Mortality
In-hospital mortality was observed in 1241 patients (7.5%). The probability of mortality is quite low on days when the Tmax is within the range of 2 to 25 °C and with a negative APmax (anomaly). For this particular outcome, only high (but not low) temperatures were associated with increased in-hospital mortality (Fig. 4), with a significantly high risk when the Tmax was above 24.3 °C (25 °C: 1.13, 1.01–1.27; 30 °C: 1.38, 1.05–1.79; 35 °C: 1.68, 1.10–2.57; 40 °C: 2.05, 1.15–3.64). Mortality also increased when the APmax (anomaly) was higher than + 3.4 hPa (+ 10 hPa: 1.21, 1.07–1.36; + 20 hPa: 1.44, 1.09–1.91; + 30 hPa: 1.73, 1.06–2.81) (Fig. 4 and Table 2). Sensitivity and subgroup analyses showed very similar results compared to the main analysis (Table 2 and Supplemental Figures 2, 4 and 5).
Adjusted effects of temperature and atmospheric pressure on in-hospital all-cause mortality of patients with AHF. Upper panels correspond to restricted cubic spline curves for predicted probabilities, and middle panels correspond to the odds ratio of mortality for every temperature and atmospheric pressure value, choosing as reference a temperature value of 20 °C and an atmospheric pressure value of 0 HPa. The bottom panel corresponds to the heat map for probability of mortality according to temperature and atmospheric pressure [inside, dots plot including the whole range of temperatures (from 0.8 to 41.6 °C) and atmospheric pressures (from − 61.7 to 69.9 hPa)]. The multivariable regression model was adjusted for median age (82 years), gender (reference Female), weekday (reference Monday), season (reference Winter), climate (reference Mediterranean), hypertension, diabetes mellitus, chronic kidney disease, coronary heart disease, cerebrovascular disease, and chronic obstructive pulmonary disease (for all risk factors, the reference was No).
The contour plot (Fig. 4) shows that the probability of in-hospital mortality by HF was (1) high (10%) when the Tmax was ~ 12 °C and the APmax(anomaly) was high (~ + 20 hPa), a typical meteorological scenario of “good weather”, from the end of autumn to early spring, due to an anticyclonic situation, and (2) maximum (~ 12%) when the Tmax was higher than 35 °C and the APmax (anomaly) was slightly negative (~ − 5 hPa).
DISCUSSION
The relationship between the variability of meteorological ambient air, temperature and mortality is a topic of worldwide interest in a changing climate with a warming trend.17 A recent global study found that the minimum mortality temperature tends to be close to the most frequent local temperature, data demonstrating human adaptability to the local climate.17,18 A recent study in Spain showed that the minimum mortality temperature has progressively increased during the last four decades (at the rate of 0.64 °C/decade), suggesting biological adaptation to climate change and/or the adoption of mitigation measures (i.e., the use of air conditioning).18 Our study specifically focused on a particular cardiovascular syndrome, HF, and investigated the potential connection between weather conditions and the severity of decompensations presented by a cohort of patients with HF. We found that the Tmax and APmax (anomaly) the day before patient ED consultation for decompensated HF were independently associated with the severity of the decompensation. Moreover, even adjusting for the two values, they could exert a different influence on disease severity, with possible different effects on the need for hospitalisation and mortality, the two outcomes investigated in the present study to assess the severity of HF decompensation.
The need for hospitalisation and mortality progressively and significantly increased from a not very high maximal temperature (around 25 °C) upwards. This means that an increase in temperatures above a certain threshold (and not only during heatwave periods) is associated with a clear increase of risk, and this should be put into the perspective of the global warming linked to climate change. Remarkably, we found a minimum probability of hospitalisation and mortality at a Tmax of ~ 20 °C, a temperature slightly lower than the minimum mortality temperature (for all natural causes) typically found in Spain, which ranges between 25 and 30 °C.18 This suggests a higher susceptibility (or less adaptive capacity) of HF patients to high temperatures than the general population or those with other diseases.
We found that, whilst a significant increase in hospitalisation was seen in patients who presented to the ED when temperatures were low, there was no increase in mortality in these patients. The apparent inconsistence between these two markers of severity was not observed for high temperatures, for which the effects on hospitalisation and mortality mirrored each other. We have no solid explanation for this. We can hypothesise that this incongruence observed for low temperatures could be because part of the decompensations during cold spells are facilitated by infections for which (bacterial) there are effective treatments. Alternatively, a lower threshold for hospitalisation during cold spells could also have accounted for the difference.
In contrast with the large number of reports analysing the impact of ambient temperature on health, the number of studies on AP are very scarce. Anticyclones (associated with high AP) typically result in stable, fine weather, with clear skies, whilst depressions (associated with low AP) are associated with cloudier, wetter, and windier conditions. Additionally, there are some relationships between AP and temperature, as high temperature is generally associated with low AP. In Spain, high temperatures are associated with meteorological scenarios characterised by a weak pressure gradient and the formation of a thermal low (i.e. relatively low pressure due to the strong heating of terrain and the consequent formation of a thermal low—meteorological terminology). This is a well-known feature on the Spanish mainland.19 However, although it is intuitive to consider anticyclonic conditions more favourable for health, we found that anticyclones were, in fact, associated, with a significant excess of hospitalisations and in-hospital deaths in patients with AHF. Our results partially disagree with those of Plavcová and Kyselý,20 who reported that sudden AP drops in winter were associated with a significant rise in hospital admissions and also with a significant excess of cardiovascular mortality in Prague (Czech Republic). It is remarkable that whilst patients can manage extreme external temperatures using air conditioning or heating devices to adjust ambient temperature to one that is more comfortable according to their own preferences/necessities, extreme AP conditions cannot be modulated. Accordingly, the impact of AP on health could be greater and more difficult to palliate than the effect of temperature. Indeed, when the AP was higher than + 30 hPa over the mean AP of the city, excesses of hospitalisation and mortality were similar to those observed with very high temperatures (40 °C). Therefore, the effects of AP on health merit thorough study in the next years.
The pathophysiology of adverse effects of extreme temperatures and AP on health is complex. For temperature, several biological mechanisms have been postulated for populations (particularly the elderly) susceptible to heat-related mortality, a condition highly present in HF patients.21 Increased blood viscosity, elevated cholesterol levels associated with higher temperatures, and a higher sweating threshold may also trigger heat-related mortality. For the particular case of HF patients, certain chronic medications such as diuretics or beta-blockers could exacerbate this disruption in homeostatic mechanisms. Furthermore, thermoregulation can also be influenced by acclimatisation: heat waves earlier in the year or affecting areas where high temperatures are unusual are more likely to impact the health of the population. Similarly, people living next to the sea are used to a very high AP, whilst people leaving at high altitudes are used to a very low AP. In this sense, it has been reported that residing at higher altitudes is associated with a lower mortality from cardiovascular diseases, and moderate altitudes would be even more protective.22
Limitations
First, as in every observational study, causal relationships cannot be inferred. Therefore, the results of the current analysis are limited by the retrospective design and should be considered as hypothesis generating. Second, several confounding factors make it difficult to study weather-related morbidity and mortality. In this sense, daily changes in temperature and AP, and other meteorological conditions such as wind, humidity or trends in changes along the immediate previous or posterior days, were not included in our models. Air pollutants were not considered in our study either. Nevertheless, an extensive review analysing the relationship between elevated temperature and mortality concluded that although some contaminants such as PM10 and PM2.5 particles and ozone can act as confounders and/or modifiers of the temperature effect, the independent negative effect of high temperatures and mortality is retained.12 Additionally, ozone is an air pollutant with a strong seasonal cycle, with high levels in summer and low levels in the other seasons, especially in the winter, and our study did not include summertime. Moreover, this study focuses on populations of urban areas, whereas ozone typically shows high levels in rural areas on a regional scale, due to the reaction of fresh nitric oxide (linked to vehicle exhaust emissions) with ozone which results in ozone titration. Therefore, we do not believe that our findings were influenced by changes in ozone levels not measured in the present study. Third, we only recorded all-cause mortality, without distinguishing between cardiovascular and non-cardiovascular causes of death. A more detailed analysis of cause of death could have contributed to better delimiting the “harvesting” effect from the inherent effect of extreme meteorological conditions in patients with AHF. Fourth, patient socioeconomic status is not included in the EAHFE Registry, and therefore, the potential effect of these socioeconomic factors is not accounted for in the present study. However, although this could be relevant, air conditioning and heat devices are present in the majority of Spanish homes, and we believe that differences in the impact of extreme external temperatures due to socioeconomic factors were minimal. Fifth, the prevalence of certain diseases, primarily outbreaks of respiratory infection, is increased during winter season and could potentially impact mortality. However, a previous study has demonstrated that HF patients decompensated by infection actually have a better prognosis than the remaining HF patients.23 Sixth, although cases with AHF related to acute coronary syndrome other than STEMI were included (non-STEMI, angina), exclusion of STEMI could partly mask the impact meteorological conditions have on outcomes, as myocardial infarction is a cardiovascular condition that is negatively impacted by extreme meteorological conditions. Finally, we did not explore the effect of very hot temperatures, as HF patients consulting the ED in the summer were not included.
Conclusions
Maximal temperatures and AP are independently associated with the severity of HF decompensations, with possible different effects on the need for hospitalisation and in-hospital mortality.
References
Tollefson J. IPCC climate report: Earth is warmer than it’s been in 125,000 years. Nature. 2021;596:171-2.
D'Ippoliti D, Michelozzi P, Marino C, et al. The impact of heat waves on mortality in 9 European cities: results from the EuroHEAT project. Environ Health 2010;9:37.
Analitis A, Katsouyanni K, Biggeri A, et al. Effects of cold weather on mortality: results from 15 European cities within the PHEWE project. Am J Epidemiol 2008 ;168:1397-408.
Redfors B, Simonato M, Chen S, Vincent F, Zhang Z, Thiele H, et al. Ambient temperature and infarct size, microvascular obstruction, left ventricular function and clinical outcomes after ST segment elevation myocardial infarction. Coron Artery Dis 2022;33:81-90.
Llorens P, Javaloyes P, Martín-Sánchez FJ, et al. Time trends in characteristics, clinical course, and outcomes of 13,791 patients with acute heart failure. Clin Res Cardiol 2018;107:897-913.
Martín-Sánchez FJ, Parra Esquivel P, Llopis García G. Thirty-day outcomes in frail older patients discharged home from the emergency department with acute heart failure: effects of high-risk criteria identified by the DEED FRAIL-AHF trial. Emergencias. 2021;33:165-73.
Aguilar Ginés S. Prognosis in heart failure: importance of physical frailty at the time of admission. Emergencias. 2020;32:147-8.
Miró Ò, Rossello X, Gil V, et al. Predicting 30-day mortality for patients with acute heart failure in the emergency department: a cohort study. Ann Intern Med 2017;167:698-705.
Ouwerkerk W, Voors AA, Zwinderman AH. Factors influencing the predictive power of models for predicting mortality and/or heart failure hospitalization in patients with heart failure. JACC Heart Fail 2014;2:429-36.
Rossello X, Bueno H, Gil V, et al. Synergistic impact of systolic blood pressure and perfusion status on mortality in acute heart failure. Circ Heart Fail. 2021; in press. https://doi.org/10.1161/CIRCHEARTFAILURE.120.007347.
Domínguez-Rodríguez A, Juárez-Prera RA, Rodríguez S, Abreu-González P, Avanzas P. Influence of meteorological conditions on hospital admission of in patients with acute coronary syndrome with and without ST segment elevation: results of the AIRACOS study. Med Int 2016;40:201-207
Alahmad B, Shakarchi A, Alseaidan M, Fox M. The effects of temperature on short-term mortality risk in Kuwait: a time-series analysis. Environ Res 2019;171:278–284.
Llauger L, Jacob J, Moreno LA, et al. Worsening renal function during an episode of acute heart failure and its relation to short- and long-term mortality: associated factors in the Epidemiology of Acute Heart Failure in Emergency Departments–Worsening Renal Function study. Emergencias. 2020;32:332-9.
Spanish Agency of Meteorology (AEMET). Accessed: 10/08/2021. Available in: http://www.aemet.es/ca/serviciosclimaticos/datosclimatologicos/atlas_climatico
Wilson EB. Probable inference, the law of succession, and statistical inference. J Am Stat Assoc 1927;22:209–12.
Harrell F. Regression Modeling Strategies. 2nd ed. New York: Springer-Verlag;2015
Yin Q, Wang J, Ren A, Li J, Guo Y. Mapping the increased minimum mortality temperatures in the context of global climate change. Nat Commun 2019;10:4
Follos F, Linares C, López-Bueno JA, et al. Evolution of the minimum mortality temperature (1983–2018): Is Spain adapting to heat? Sci Total Environ 2021;784:147233
Zeka A, et al. The association of cold weather and all-cause and cause-specific mortality in the island of Ireland between 1984 and 2007. Environ Health 2014;13:104.
Plavcová E, Kyselý J. Effects of sudden air pressure changes on hospital admissions for cardiovascular diseases in Prague, 1994-2009. Int J Biometeorol 2014;58:1327-37.
Astrand PO, Rodahl K, Dahl HA, Stromme SB. Textbook of Work Physiology: Physiological Bases of Exercise (4th edition). Canada: McGraw-Hill;2003.
Burtscher M. Effects of living at higher altitudes on mortality: a narrative review. Aging Dis 2013;5:274-80
Miró Ò, Takagi K, Gayat É, et al. Time-pattern of adverse outcomes after an infection-triggered acute heart failure decompensation and the influence of early antibiotic administration and hospitalisation: results of the PAPRICA-3 study. Clin Res Cardiol 2020;109:34-45.
Acknowledgements
This work was partially supported by competitive grants from the Instituto de Salud Carlos III supported with funds from the Spanish Ministry of Health and FEDER (PI18/00393). The ICA-Research Group has received unrestricted funding from Novartis and Orion Pharma. We appreciate the high professionalism of Alicia Díaz in the data management of the EAHFE Registry. The design of the study, patient inclusion, data analysis, discussion and final conclusions were exclusively carried out by the authors with no participation of the granters.
Members of the EAHFE research group: Marta Fuentes, Cristina Gil (Hospital Universitario de Salamanca), Héctor Alonso, Enrique Pérez-Llantada (Hospital Marqués de Valdecilla de Santander), Francisco Javier Martín-Sánchez, Guillermo Llopis García, Mar Suárez Cadenas (Hospital Clínico San Carlos de Madrid), Òscar Miró, Víctor Gil, Rosa Escoda, Sira Aguiló, Carolina Sánchez (Hospital Clínic de Barcelona), Javier Millán (Hospital Politénic La Fe de Valencia), José Pavón (Hospital Dr. Negrín de Las Palmas de Gran Canaria), Antonio Noval (Hospital Insular de Las Palmas de Gran Canaria), María Luisa López-Grima, Amparo Valero, María Ángeles Juan (Hospital Dr. Peset de Valencia), Alfons Aguirre, Maria Angels Pedragosa, Silvia Mínguez Masó (Hospital del Mar de Barcelona), María Isabel Alonso, Francisco Ruiz (Hospital de Valme de Sevilla), José Miguel Franco (Hospital Miguel Servet de Zaragoza), Ana Belén Mecina (Hospital de Alcorcón de Madrid), Josep Tost, Marta Berenguer, Ruxandra Donea (Consorci Sanitari de Terrassa), Susana Sánchez Ramón, Virginia Carbajosa Rodríguez (Hospital Universitario Rio Hortega de Valladolid), Pascual Piñera, José Andrés Sánchez Nicolás (Hospital Reina Sofía de Murcia), Raquel Torres Garate (Hospital Severo Ochoa de Madrid), Aitor Alquézar-Arbé, Miguel Alberto Rizzi, Sergio Herrera (Hospital de la Santa Creu y Sant Pau de Barcelona), Javier Jacob, Alex Roset, Irene Cabello, Antonio Haro (Hospital Universitari de Bellvitge de Barcelona), Fernando Richard, José María Álvarez Pérez, María Pilar López Diez (Hospital Universitario de Burgos), Pablo Herrero Puente, Joaquín Vázquez Álvarez, Belén Prieto García, María García García, Marta Sánchez González (Hospital Universitario Central de Asturias de Oviedo), Pere Llorens, Patricia Javaloyes, Inmaculada Jiménez, Néstor Hernández, Begoña Espinosa, Adriana Gil, Francisca Molina, Tamara García (Hospital General de Alicante), Juan Antonio Andueza (Hospital General Universitario Gregorio Marañón de Madrid), Rodolfo Romero (Hospital Universitario de Getafe de Madrid), Martín Ruíz, Roberto Calvache (Hospital de Henares de Madrid), María Teresa Lorca Serralta, Luis Ernesto Calderón Jave (Hospital del Tajo de Madrid), Beatriz Amores Arriaga, Beatriz Sierra Bergua (Hospital Clínico Lozano Blesa de Zaragoza), Enrique Martín Mojarro, Brigitte Silvana Alarcón Jiménez (Hospital Sant Pau i Santa Tecla de Tarragona), Lisette Travería Bécquer, Guillermo Burillo (Hospital Universitario de Canarias de Tenerife), Lluís Llauger García, Gerard Corominas LaSalle. (Hospital Universitari de Vic de Barcelona), Carmen Agüera Urbano, Ana Belén García Soto, Elisa Delgado Padial (Hospital Costa del Sol de Marbella de Málaga), Ester Soy Ferrer, María Adroher Múñoz (Hospital Josep Trueta de Girona). José Manuel Garrido (Hospital Virgen Macarena de Sevilla), Francisco Javier Lucas-Imbernón (Hospital General Universitario de Albacete), Rut Gaya (Hospital Juan XXIII de Tarragona), Carlos Bibiano, María Mir, Beatriz Rodríguez (Hospital Infanta Leonor de Madrid), José Luis Carballo (Complejo Hospitalario Universitario de Ourense), Esther Rodríguez-Adrada, Belén Rodríguez Miranda, Monika Vicente Martín (Hospital Rey Juan Carlos de Móstoles de Madrid). Pere Coma Casanova, Joan Espinach Alvarós (Hospital San Joan de Deu de Martorell, Barcelona).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Òscar Miró, Miguel Benito Lozano, and Pedro Lopez-Ayala equally contributed to this manuscript and should be considered as first authors.
Supplementary Information
ESM 1
(PDF 749 kb)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Miró, Ò., Benito-Lozano, M., Lopez-Ayala, P. et al. Influence of Meteorological Temperature and Pressure on the Severity of Heart Failure Decompensations. J GEN INTERN MED 38, 600–609 (2023). https://doi.org/10.1007/s11606-022-07743-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07743-7